This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box"
DR JATIN SHARMA
Roll no. 56
A 20 YEAR OLD FEMALE WITH FEVER AND HEADACHE
Date of admission : 7-2-23
Presenting complaints :
Fever since 1 week
Vomitings since 1 week
Dryness of mouth since 1 week
Chest pain since 1 week
Palpitations since 1 week
Shortness of breath since 1 week
History of presenting illness:
Patient was apparently asymptomatic one week back the he developed fever of high grade with chills, insidious in onset, gradually progressive, not relieved on taking medication.
Associated with vomitings contained food particles, non bilious, non projectile, 3-4 episodes/day. Associated with dryness of mouth. H/o chest pain, left sided, pricking type, non radiating associated with sob grade 3, insidious in onset gradually progressive. No h/o orthopnea.
H/o blurring of vision present
No h/o pain abdomen
No h/o dizziness, altered sensorium
No h/o decresed urine output
Ophthalmologist opinion taken on 8-2-23. Impression : no diabetic retinopathy changes noted
Past history :
K/c/o DM I since 8 yrs (diagnosed at the age of 17yrs) and on biphasic isophene insulin injection( 30% soluble insulin and 70% isophene insulin) 24U in the mrng and 20U in the night.
Not a k/c/o HTN / Asthma / CAV / CAD
Personal history :
Sleep: adequate
Appetite: normal
Diet: mixed
Bowel and bladder movements: normal
Addictions: none
Family history :
No similar complaints in family
General examination :
Patient Is conscious, coherent, cooperative moderately built and well nourished
pallor - Absent
icterus - Absent
clubbing - Absent
cyanosis - Absent
lymphadenopathy - Absent
Edema - Absent
Vitals:
TEMP-96.5 F
PR-82/MIN
RR-14/MIN
BP-110/70MMHG
SPO2-99% AT ROOM AIR
GRBS-197MG%.
Systemic examination :
CVS - S1S2 present, no murmur
RS - Bilateral air entry present, trachea central in position
CNS - Higher mental functions intact
P/A - Soft, non tender
Clinical images with investigations:
ECG DONE ON PRESENTATION 8-2-23
REPEAT ECG 8-2-23
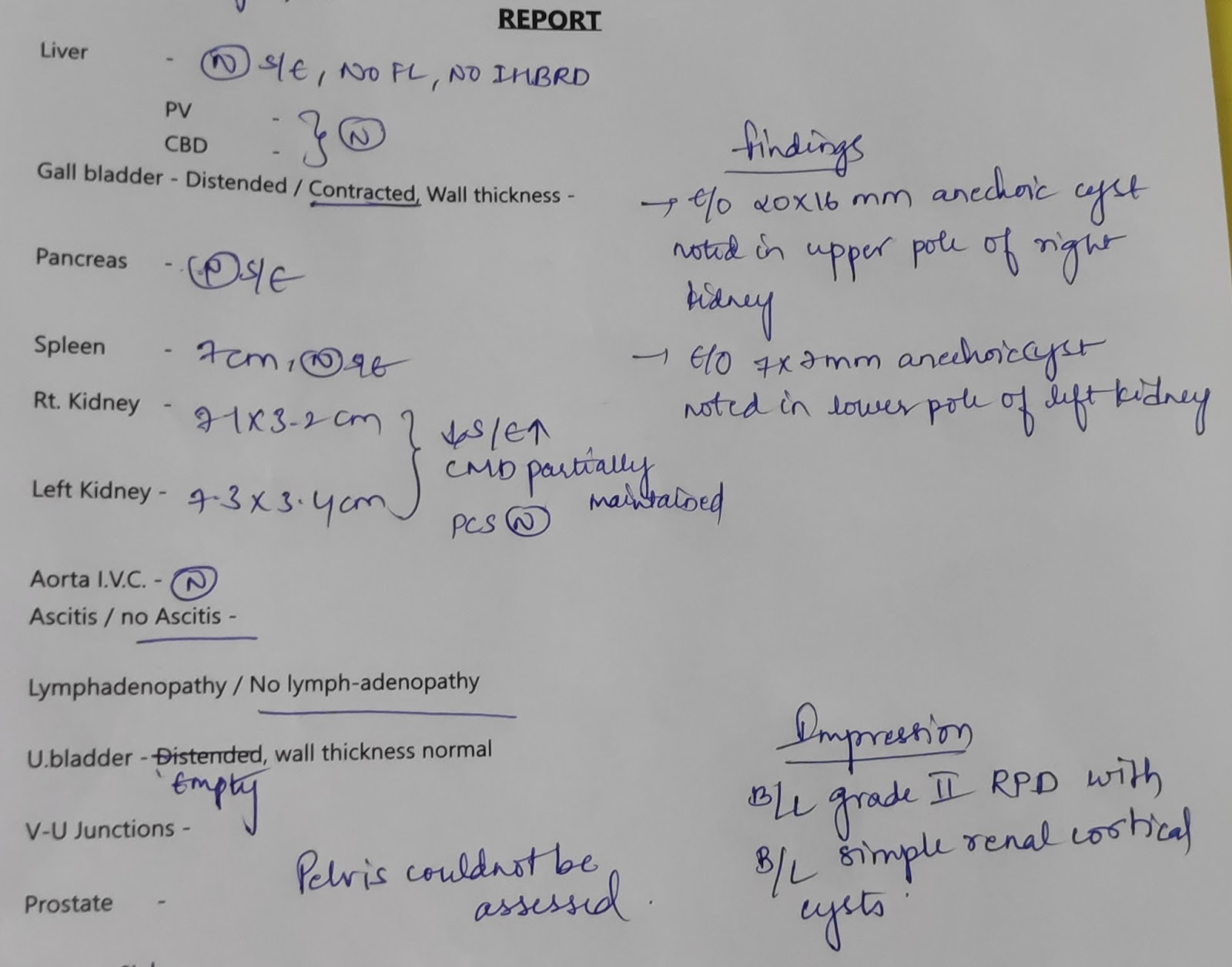
USG ABDOMEN DONE ON 8-2-23
BLOOD AND URINE INVESTIGATIONS
Diagnosis :
DIABETIC KETOACIDOSIS(RESOLVED) WITH OLD INFERIOR WALL MI WITH K/C/O TYPE I DM SINCE 9YRS WITH DIABETIC NEPHROPATHY
Treatment :
* IV FLUIDS NS@75ML/HR
5% DEXTROSE IF GRBS <= 250MG/DL
* HUMAN ACTRAPID INSULIN INFUSION ( 1ML +39 ML NS) @ 3ML/HR BASED ON GRBS
* TAB ECOSPRIN GOLD 75/75/10MG PO HS
* GRBS MONITORING HOURLY
* STRICT I/O CHARTING.
* VITALS MONITORING 2ND HRLY.
SOAP NOTES :
Date : 08/02/23
ICU
Unit 2
DR..AASHITHA SR
DR.PRADEEP PGY3
DR. VINAY PGY3
DR.NARASIMHA PGY2
DR.AJAY PGY1
DR.PARCHETHAN PGY1
DR.JATIN INTERN
DR.SANTHOSH INTERN
S
STOOLS NOT PASSED
NO FEVER SPIKE
O
PATIENT IS CONSCIOUS COHERENT COOPERATIVE .
VITALS:
TEMP-96. 5F
PR-82/MIN
RR-14/MIN
BP-110/70MMHG
SPO2-99% AT ROOM AIR
GRBS-197MG%.
SYSTEMIC EXAMINATION:
P/A- SOFT NON TENDER
CVS-S1 S2 PRESENT,NO MURMURS
RS-B/L AIR ENTRY PRESENT,NVBS HEARD
CNS-NAD
A:
DIABETIC KETOACIDOSIS WITH OLD INFERIOR WALL MI WITH K/C/O TYPE I DM SINCE 9YRS WITH DIABETIC NEPHROPATHY
P:
* IV FLUIDS NS@75ML/HR
5% DEXTROSE IF GRBS <= 250MG/DL
* HUMAN ACTRAPID INSULIN INFUSION ( 1ML +39 ML NS) @ 3ML/HR BASED ON GRBS
* TAB ECOSPRIN GOLD 75/75/10MG PO HS
* GRBS MONITORING HOURLY
* STRICT I/O CHARTING.
* VITALS MONITORING 2ND HRLY.
Date : 09/02/23
ICU
Unit 2
DR..AASHITHA SR
DR.PRADEEP PGY3
DR. VINAY PGY3
DR.NARASIMHA PGY2
DR.AJAY PGY1
DR.PARCHETHAN PGY1
DR.JATIN INTERN
DR.SANTHOSH INTERN
S
STOOLS NOT PASSED
NO FEVER SPIKE
O
PATIENT IS CONSCIOUS COHERENT COOPERATIVE .
VITALS:
TEMP- AFEBRILE
PR-82/MIN
RR-18/MIN
BP-110/70MMHG
SPO2-98% AT ROOM AIR
GRBS-216MG%.
SYSTEMIC EXAMINATION:
P/A- SOFT NON TENDER
CVS-S1 S2 PRESENT,NO MURMURS
RS-B/L AIR ENTRY PRESENT,NVBS HEARD
CNS-NAD
A:
DIABETIC KETOACIDOSIS(RESOLVED) WITH OLD INFERIOR WALL MI WITH K/C/O TYPE I DM SINCE 9YRS WITH DIABETIC NEPHROPATHY
P:
* IVF NS @ 75ML/HR
* INJ HAI 14U---14U---14U
INJ NPH 20U---×---20U
* TAB ECOSPRIN GOLD 75/75/10MG PO HS
* TAB TELMA 40MG PO OD
* GRBS CHARTING
* STRICT I/O CHARTING.
* VITALS MONITORING